Role of the Affordable Care Act
 In New Mexico, the concept of a “Health Commons” as a one-stop-shop for care was created which integrated in one clinic the services of primary care, behavioral health, oral health, social services and public health with clinic/community liaisons (community health workers). Two of the Health Commons models are housed in a federally qualified community health center and, via an MOU with the UNM HSC, serve as continuity clinical training sites for residents in Family Medicine. Those clinics were very popular training sites in primary care and have attracted the most residency graduates to practice in those locations, thus becoming de facto “Teaching Community Health Centers.”
In New Mexico, the concept of a “Health Commons” as a one-stop-shop for care was created which integrated in one clinic the services of primary care, behavioral health, oral health, social services and public health with clinic/community liaisons (community health workers). Two of the Health Commons models are housed in a federally qualified community health center and, via an MOU with the UNM HSC, serve as continuity clinical training sites for residents in Family Medicine. Those clinics were very popular training sites in primary care and have attracted the most residency graduates to practice in those locations, thus becoming de facto “Teaching Community Health Centers.”
Section 5405- A Primary Care Extension Service
 As part of the creation of the ACA, the staff of the Senate Health, Education, Labor and Pensions (HELP) Committee, the committee tasked with writing the bill, invited the Health Extension programs from New Mexico and Oklahoma and champions of the concept from the American Association of Family Physicians and UC-San Francisco to contribute ideas for writing a piece of the legislation entitled the Primary Care Extension Program. Drafts were written and this group invited to meet the HELP Committee staff helped edit and rework the concept which eventually became Section 5405, the Primary Care Health Extension Program. While extension programs in different states followed different models and had different scopes, the ACA section focused on those aspects of Health Extension that were related to primary care in light of the significant role the ACA developers saw for primary care in the new healthcare system.
As part of the creation of the ACA, the staff of the Senate Health, Education, Labor and Pensions (HELP) Committee, the committee tasked with writing the bill, invited the Health Extension programs from New Mexico and Oklahoma and champions of the concept from the American Association of Family Physicians and UC-San Francisco to contribute ideas for writing a piece of the legislation entitled the Primary Care Extension Program. Drafts were written and this group invited to meet the HELP Committee staff helped edit and rework the concept which eventually became Section 5405, the Primary Care Health Extension Program. While extension programs in different states followed different models and had different scopes, the ACA section focused on those aspects of Health Extension that were related to primary care in light of the significant role the ACA developers saw for primary care in the new healthcare system.
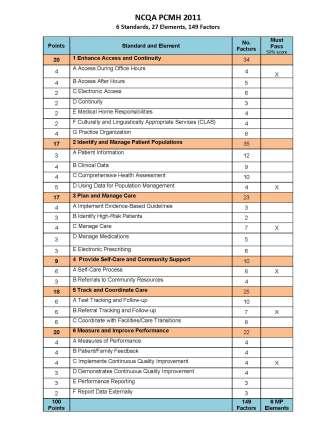
 Section 5405 was intended to assist primary care providers to implement a patient-centered medical home to improve the accessibility, quality, and efficiency of primary care services. It would accomplish this through the local deployment of community-based practice improvement facilitators and health connectors (“Health Extension Agents”). And states receiving funding through this section could implement discretionary activities beyond practice facilitation roles such as “collaborating with local health departments, community health centers, tribes and tribal entities and other community agencies to identify community health priorities and local health workforce needs, and participate in community-based efforts to address the social and primary determinants of health, strengthen the local primary care workforce, and eliminate health disparities.”
Section 5405 was intended to assist primary care providers to implement a patient-centered medical home to improve the accessibility, quality, and efficiency of primary care services. It would accomplish this through the local deployment of community-based practice improvement facilitators and health connectors (“Health Extension Agents”). And states receiving funding through this section could implement discretionary activities beyond practice facilitation roles such as “collaborating with local health departments, community health centers, tribes and tribal entities and other community agencies to identify community health priorities and local health workforce needs, and participate in community-based efforts to address the social and primary determinants of health, strengthen the local primary care workforce, and eliminate health disparities.”
The ACA authorized the Agency for Healthcare Research and Quality (AHRQ) to create the national Primary Care Extension Program. Federal funding for this section would be allocated through AHRQ. Though Congress authorized Section 5405, it did not appropriate funds for it. However, AHRQ mobilized $4 million of its own resources to fund four states directly to develop Primary Care Health Extension and for each to disseminate their model to at least three other states.
The PCEP Model
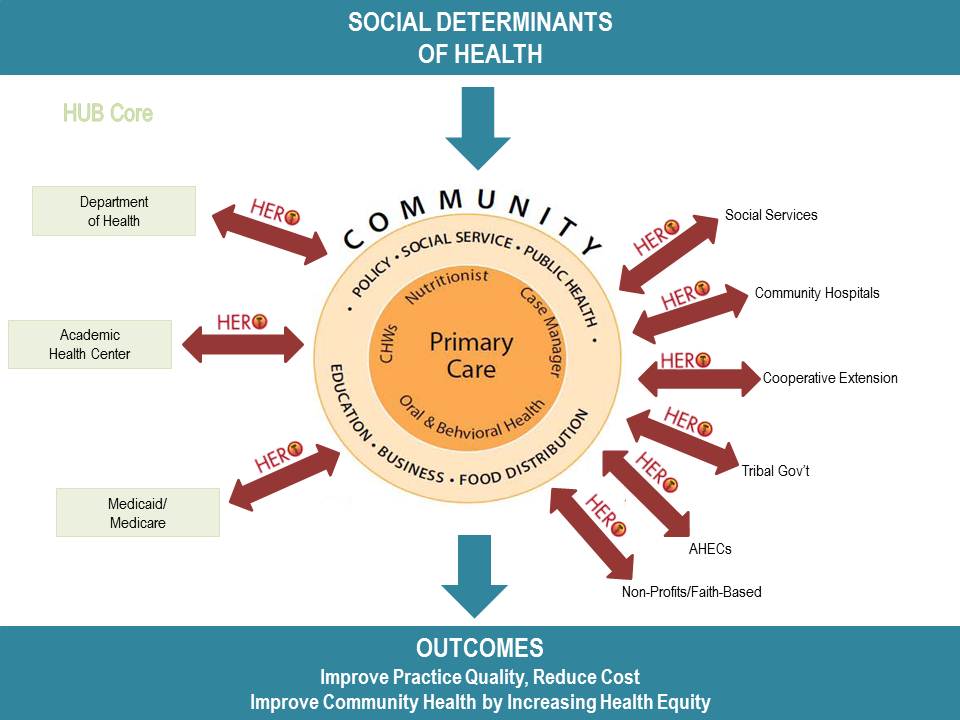
In NM, the HEROs program is an established, unique, replicable model addressing priority community health problems with resources from universities and agencies. Health Extension is a method of helping primary care practices overcome barriers to transformation by sharing common resources. HEROs connects resources of the academic health center, public health and other state agencies, and the state’s predominantly rural, minority, and underserved communities that depend on primary care practices for immediate access to health care.
The fundamental strategy to address the challenges to primary care infrastructure and practice is the concept of Health Extension as a community-based, state-wide, but university-linked network of agents that can assist primary care practices with the best evidence-based practices to support the provision of quality care and practice transformation. These resources are important for the transformation process since many practices do not have the capacity nor could they afford to develop and support these developmental milestones on their own.
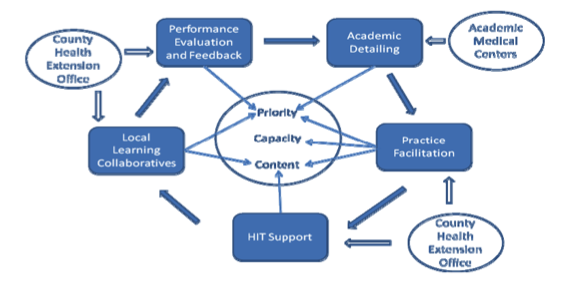
The model of how HEROs functions as a “Primary Care Extension Program” is demonstrated below:
In Oklahoma, it is recognized that the transformation of primary care cannot be accomplished by focusing entirely on practices. Links between primary care and subspecialists, hospitals, home health and hospice agencies, public and mental health departments, and community resources must be strengthened. Because health and illness are multi-determinant, health improvement requires community wide collaboration and multi-level interventions. Problems like obesity,
inactivity, and smoking cannot be solved without community-wide collaboration. Even problems like hypertension might be better addressed at a community level. In addition, small and medium-sized primary care practices will not be able to afford to employ, train, and supervise the staff required to support many components of the PCMH including care management, registry management, and patient education. Their survival will depend therefore on their ability to share key personnel and resources across practices. Over the past decade, Oklahoma researchers have contributed to a body of knowledge that suggests that the combination of performance measurement with feedback, academic detailing, practice facilitation, and HIT support, with or without local learning collaboratives, consistently enhances implementation of specific evidence-based practices and facilitates transformative changes in small to medium-sized primary care practices.
Application of Health Extension to Primary Care Transformation
Health extension can help gauge the help practices need and want
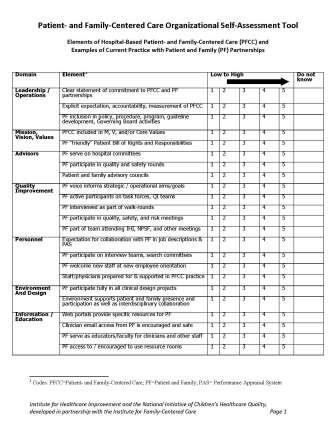
Health extension can survey the practice regarding readiness for change and suggest where to start along the path to practice transformation– click below for some sample assessment tools: