The Movement toward Patient-Centered Medical Home
 The movement towards Patient-Centered Medical Homes (PCMHs) is a growing national expectation of primary care practices. Practices are expected to ensure that each patient receives continuous care from a clinician; that each clinician takes the lead when referring the patient to specialists; that each practice make meaningful use of electronic health records; and that every patient and family actively participates in their own care. However, aside from federal support for adopting electronic health records and implementing their meaningful use, most primary care practices will not receive external funding to implement other vital components of healthcare reform including the transformation to PCMH. They will need assistance in reallocating existing scarce resources to implement needed change; in finding relevant primary care demonstrations conducted elsewhere; and guidance on how they can adapt different aspects of successful models in their own practice.
The movement towards Patient-Centered Medical Homes (PCMHs) is a growing national expectation of primary care practices. Practices are expected to ensure that each patient receives continuous care from a clinician; that each clinician takes the lead when referring the patient to specialists; that each practice make meaningful use of electronic health records; and that every patient and family actively participates in their own care. However, aside from federal support for adopting electronic health records and implementing their meaningful use, most primary care practices will not receive external funding to implement other vital components of healthcare reform including the transformation to PCMH. They will need assistance in reallocating existing scarce resources to implement needed change; in finding relevant primary care demonstrations conducted elsewhere; and guidance on how they can adapt different aspects of successful models in their own practice.
Health extension is an established, unique, replicable model addressing priority community health problems with resources from universities and agencies. Health Extension is a method of helping primary care practices overcome barriers to transformation by sharing common resources. It connects resources of the academic health center, public health and other state agencies, to a state’s rural, minority, and underserved communities that depend on primary care practices for immediate access to health care.
PCMH- What’s in it for small practices?
 The majority of primary care practitioners work in small or moderate sized practices (10 or less primary care providers). Adoption of a PCMH is difficult for many small, independent primary care sites that are often isolated from one another and in turn are further isolated from specialty and support services required for comprehensive care of various and complex conditions. Health extension offers an opportunity to share resources across practices and geographic distances and to help small practices meet their functional requirements as medical homes.
The majority of primary care practitioners work in small or moderate sized practices (10 or less primary care providers). Adoption of a PCMH is difficult for many small, independent primary care sites that are often isolated from one another and in turn are further isolated from specialty and support services required for comprehensive care of various and complex conditions. Health extension offers an opportunity to share resources across practices and geographic distances and to help small practices meet their functional requirements as medical homes.
Supporting Readiness for Change
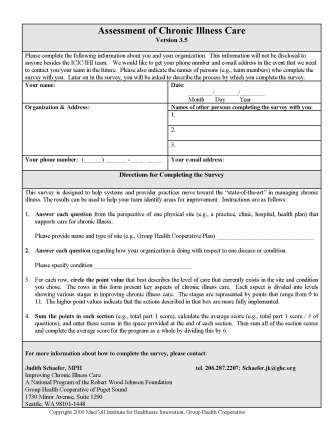
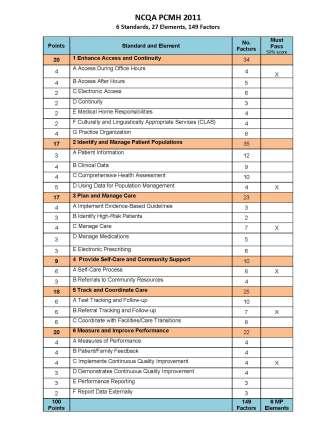
Many organizations offer models assessing primary care practice readiness for change toward PCMH. One of the most organized is from Transformed, a subsidiary of the American Academy of Family Physicians. The components of the Transformed model include an on-line assessment applicable for clinical staff, office staff, and residency programs; a transformation package specially designed for small practices; medical home facilitation offering an on-site practice facilitator; a baseline practice assessment via surveys, interviews, phone conversations and e-mail communications with key practice staff.
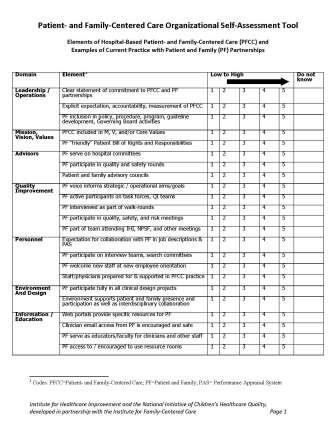
Group Health Cooperative offers an Assessment of Chronic Illness Care tool. The survey helps systems and provider practices move toward the “state-of-the-art” in managing chronic illness. The results can help clinic teams identify areas for improvement. Click on the image below to access the assessment.
Building Capacity for Technical & Adaptive Change
 Strengthened primary care regarding its quality and its service to community health is of vital interest to our society. It is especially the case in the current environment where resources are increasingly constrained, the supply of primary care physicians and providers cannot meet the demand for those seeking a medical home. So it is imperative that, as an effective way to build capacity, many parallel, poorly communicating systems of health care come together and coordinate their efforts, thereby providing a more efficient, more effective health system with less duplication of services and less neglect of important health needs of our patients and their communities. Health extension can draw upon and pull together the following organizations:
Strengthened primary care regarding its quality and its service to community health is of vital interest to our society. It is especially the case in the current environment where resources are increasingly constrained, the supply of primary care physicians and providers cannot meet the demand for those seeking a medical home. So it is imperative that, as an effective way to build capacity, many parallel, poorly communicating systems of health care come together and coordinate their efforts, thereby providing a more efficient, more effective health system with less duplication of services and less neglect of important health needs of our patients and their communities. Health extension can draw upon and pull together the following organizations:
Practices have Different Needs
Practices are often so overwhelmed with patients and feel stretched in terms of staff and resources, so they need help and guidance–which EMR to choose? How to achieve meaningful use? How and where to recruit personnel? How to offer continuing education for their staff? How to keep current with the best evidence of practice when information overload is manifested by the growing pile of unread journals?…
Health Extension Role in Primary Care Practice Transformation
Health extension agents can help gauge the help practices need and want
Health extension agents can survey the practice regarding readiness for change and suggest where to start along the path to practice transformation– click below for some sample assessment tools:
Related Literature & Tools