Lead State: Oklahoma
Oklahoma’s health statistics are among the worst in the nation. Some of the reasons for this are clear. One-third of premature deaths in the U.S. are the result of lack of physical activity, poor eating habits, use of tobacco products, and excessive ingestion of alcohol, and more Oklahomans engage in these unhealthy behaviors than do people in most other states.
In a 2011 government report, the quality of health care provided in Oklahoma was rated as “weak” compared to other states, particularly in the area of chronic disease management. The rate of preventable hospitalizations in Oklahoma is significantly higher than the national average. Poor health and quality of health care result in increased health care costs and health insurance premiums and adversely impact worker productivity and Oklahoma’s ability to recruit and retain new businesses.
The Importance of Primary Care
The overall quality of care in any health care system is directly associated with the strength of its primary care network. Currently, Oklahoma has one of the lowest proportions of primary care clinicians per capita in the U.S. The need to adjust to the changing epidemiology of illnesses (acute to chronic), keep up with the accelerated pace of scientific advances, adopt information technologies, meet higher societal expectations, and meet increasing documentation requirements, primary care practices are under-resourced and overwhelmed. These realizations have resulted in state and nationwide quality improvement (QI) and payment reform efforts guided by the Patient-Centered Medical Home (PCMH) model and the Comprehensive Primary Care Initiative. These efforts have revealed how much change is needed and how difficult it is to effect change. To date, most successful PCMH initiatives have occurred in large health systems. Small practices, which make up more than 40% of practices in Oklahoma, are much less able to employ, train, and supervise the additional staff required to support care management, population management, and patient self management support. Their survival will depend upon their ability to access and probably share personnel and other resources, and they will need support to facilitate the organizational process changes required.
Connecting Primary Care, Public Health, Mental Health and Community Initiatives
Much has been done in recent years to try to address Oklahoma’s health and primary health care challenges. Research conducted by University of Oklahoma faculty and others have led to the development of effective approaches to quality improvement in primary care practices. Turning Point Partnerships involving local stakeholder groups have been developed in all 77 counties and nurtured by the State Department of Health. These efforts must be continued and strengthened, and, whenever possible, be better aligned. Reducing the major risk factors for poor health will require much closer collaborations between primary care, public health, mental health, and community-based organizations. Consistent with the World Health Organization’s of primary health care, a much broader concept than primary medical care, Oklahoma has therefore chosen to focus on improving, “primary health care,” a World Health Organization term that is broader than “primary care.”
A Solution
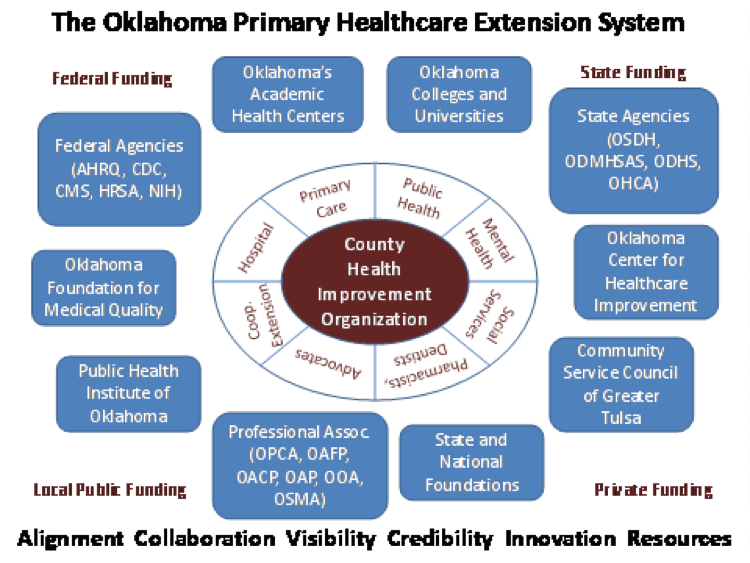
The proposed primary healthcare extension system (OPHES) will improve the quality of primary health care available to Oklahomans, reduce the cost of care and health insurance premiums, and improve the health of the population. Greater visibility and better alignment of local initiatives will increase their efficiency and effectiveness and leverage funding from a wider range of sources. OPHES is made up of independent certified county health improvement organizations (CHIOs) coordinated by the Public Health Institute of Oklahoma and the Community Services Council with support from the Oklahoma Primary Healthcare Improvement Cooperative (OPHIC) and in collaboration with the Turning Point Field Consultants employed by the Oklahoma State Department of Health.
County Health Improvement Organizations (CHIOs)
A certification program offered by PHIO strengthens and increases the visibility of existing Turning Point Partnerships and/or other community-based coalitions (e.g. Sooner Success, Wellness Now, etc.) by helping them to become 501c3 non-profit (“neutral convener”) organizations, putting them in a better position to attract both public and private funding. CHIOs will also be in a position to hire or contract with care managers, community health workers, mental health professionals, and others who will expand the capabilities of the primary care practices, working collaboratively with them and with other community organizations.
The Public Health Institute of Oklahoma (PHIO)
PHIO is a non-profit organization established in 2004 to “promote health through collaboration among government, academia, and communities.” Its Board of Directors (BOD) includes representatives from public health, primary care, the academic medical centers, hospitals, the Oklahoma Health Care Authority (OHCA), and community-based organizations. PHIO serves as the state hub for the extension system, managing certification of the CHIOs, serving as temporary fiscal agent for those awaiting independent non-profit status, maintaining the OPHES website, and communicating the availability of resources.
The Community Services Council (CSC)
CSC is a non-profit organization that serves an incubator for emerging non-profits and helps launch large initiatives throughout the state. It assists the CHIOs with organizational development and grant writing, and it also helps connect them to available resources. Through contracts with OPHIC, it helps train and deploy academic detailers.
Oklahoma Primary Healthcare Improvement Cooperative (OPHIC)
OPHIC is an administrative unit within the Oklahoma Clinical and Translational Science Institute at the University of Oklahoma Health Sciences Center. Its focus is on the dissemination and implementation of evidence-based practices in primary care. Its usual approach involves providing performance evaluation and feedback, academic detailing, practice facilitation, and IT support on-site to practices.

Land Area: 68,595 miles
Population: 3,814,820
Persons per square mile: 54.7
Median household: $44,287
Below poverty level: 16.3%
Collaborators within Oklahoma

Daniel Duffy, MD
Director, Oklahoma Primary Healthcare Improvement Cooperative
Email: Daniel-Duffy@ouhsc.edu

Steven Crawford, MD
Co-Directore, Oklahoma Primary Healthcare Improvement Cooperative
Email: Steven-Crawford@ouhsc.edu
James W. Mold, MD, MPH
Consultant
Email: James-Mold@ouhsc.edu

Jill Hazeldine
Executive Director, Public Health Institute of Oklahoma
Email: Jill@publichealthok.org

Laura Ross-White
Community Services Council
Email: LRWhite@csctulsa.org
Find out more about the states participating in health extension around the country:
 Lead States (funded through AHRQ IMPaCT grants)
Lead States (funded through AHRQ IMPaCT grants)
 Learning Community Participants
Learning Community Participants