Origins of the Health Extension Concept
This video introduction describes in general terms how the health extension concept was born. For a more detailed history, the following presentation from the first national primary care extension conference in Oklahoma may prove helpful:
For further introduction, the health extension program in Pennsylvania has also created the following video:
History of Health Extension in New Mexico
 The interventions employed by Health Extension Agents embody a set of service innovations created in New Mexico over the last dozen years. These were meant to address challenges common to other states as well– mix of underserved rural and urban populations, high uninsured rate, and large ethnic minority population with poor access to primary care, behavioral health and oral health.
The interventions employed by Health Extension Agents embody a set of service innovations created in New Mexico over the last dozen years. These were meant to address challenges common to other states as well– mix of underserved rural and urban populations, high uninsured rate, and large ethnic minority population with poor access to primary care, behavioral health and oral health.
Click below to hear a vignette from Charlie Alfero, a CEO from a local health system in one of the first communities to connect with health extension in southwestern New Mexico.
Place-Based Priorities: Many Approaches to Health Extension
Four states are leading the health extension movement nationally: New Mexico, North Carolina, Oklahoma and Pennsylvania. In addition, 13 other states comprise a learning community, adapting the lessons learned in the lead states to their own place-based circumstances. Within this learning community, states are sharing their own approaches, contributing their complementary strengths so that each state is learning from the others, building a new and broader Health Extension model.
Click on the map images below to learn more about how health extension is developing in each state.
LEAD STATES
LEARNING COMMUNITY
Role of the Affordable Care Act
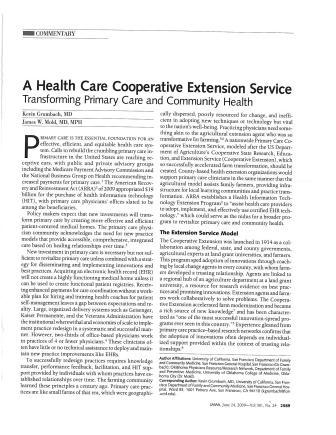
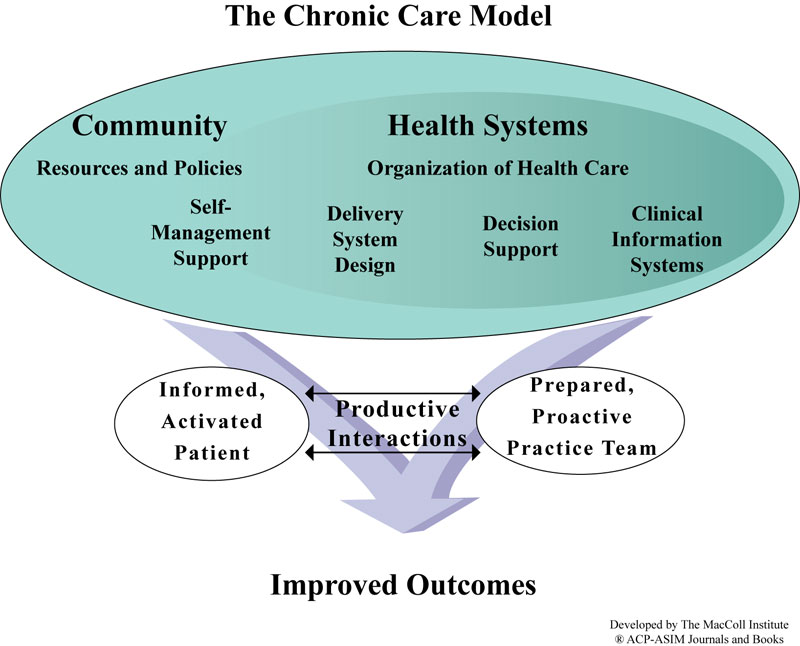
Wide-scale implementation of new models of care, such as the Chronic Care Model, reveals lessons about the diffusion of innovation. Risk-acceptant, financially sound practices with close contact to scientific resources and interaction with other innovators are likely to be the first and most successful adopters. (Rogers, 1962) Yet, the primary care landscape is dotted with isoloated, small and solo practices; more than 80% of primary care practices have five or fewer clinicians. Compared to the integrated systems in which new models of care have been successfully implemented, small and solo practices operate under greater time constraints, employ fewer staff, have narrower margins, and little time for reflection and relationship building.
Recognizing the needs of small practices for help in transforming to new models of care, the ACA authorized the Agency for Healthcare Research and Quality (AHRQ) to create a national Primary Care Extension Program (PCEP). The goal of the program is to improve community health by deploying community-based health “connectors,” known as Health Extension Agents, to increase primary care providers’ knowledge and use of preventive medicine, health promotion, chronic dieseae management, behavioral health, and evidence-based medicine.
Change within the Primary Care Practice is Not Enough
The PCEP has thus evolved to address the needs of community health as well as the needs of patients within primary care practices. In many states, the model has grown as an important vehicle for improving the quality of primary care practices while addressing the health of communities served by those practices.

The Shifting Health System Paradigm
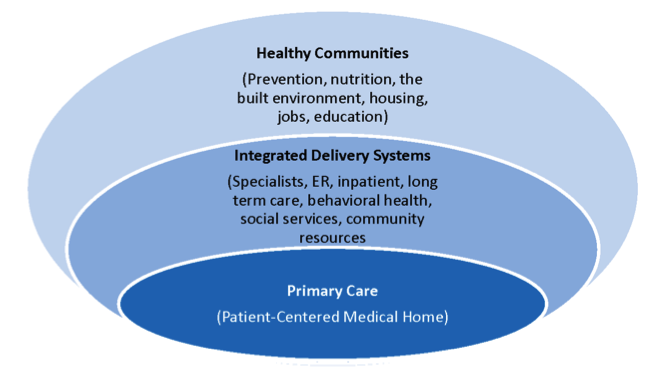
The Affordable Care Act and the Triple Aim place primary care front and center, as the foundation of a new health care delivery system. Primary care alone, however, is an island unless it is seamlessly knit together with other medical, social and community services. Payment reform, moving toward paying for outcomes and freeing providers from the tyranny of fee-for-service, offers the potential to invest resources in mitigating the upstream causes of illness.
This progression—from the delivery of narrowly defined medical services to addressing the social determinants of health—defines a vision and evolutionary path for primary care. The role of a primary care extension program—or of primary care technical assistance—is to accelerate and facilitate the progression of a primary care practice along this evolutionary path.
Thus, the first task is to assist in building strong, sustainable and effective models of primary care practice—currently defined by the precepts of the patient-centered medical home.
The second task is to assure the integration of that practice into the larger system of medical and social services and community resources that are needed for effective care of a patient or family.
The third task is to examine the underlying causes of illness as they appear in that practice’s population or community and to intervene as appropriate, in concert with other organizations who have the health of the community at heart. In underserved communities, federally qualified health centers are a major primary care resource and this evolutionary path takes them back to their origins in community-oriented primary care and the notion that it is ultimately the community—and not necessarily the individual walking into the practice—that is the patient.
It is in Tasks 2 and 3 that the synergy with the Cooperative Extension Service is at its strongest.