Technical Assistance
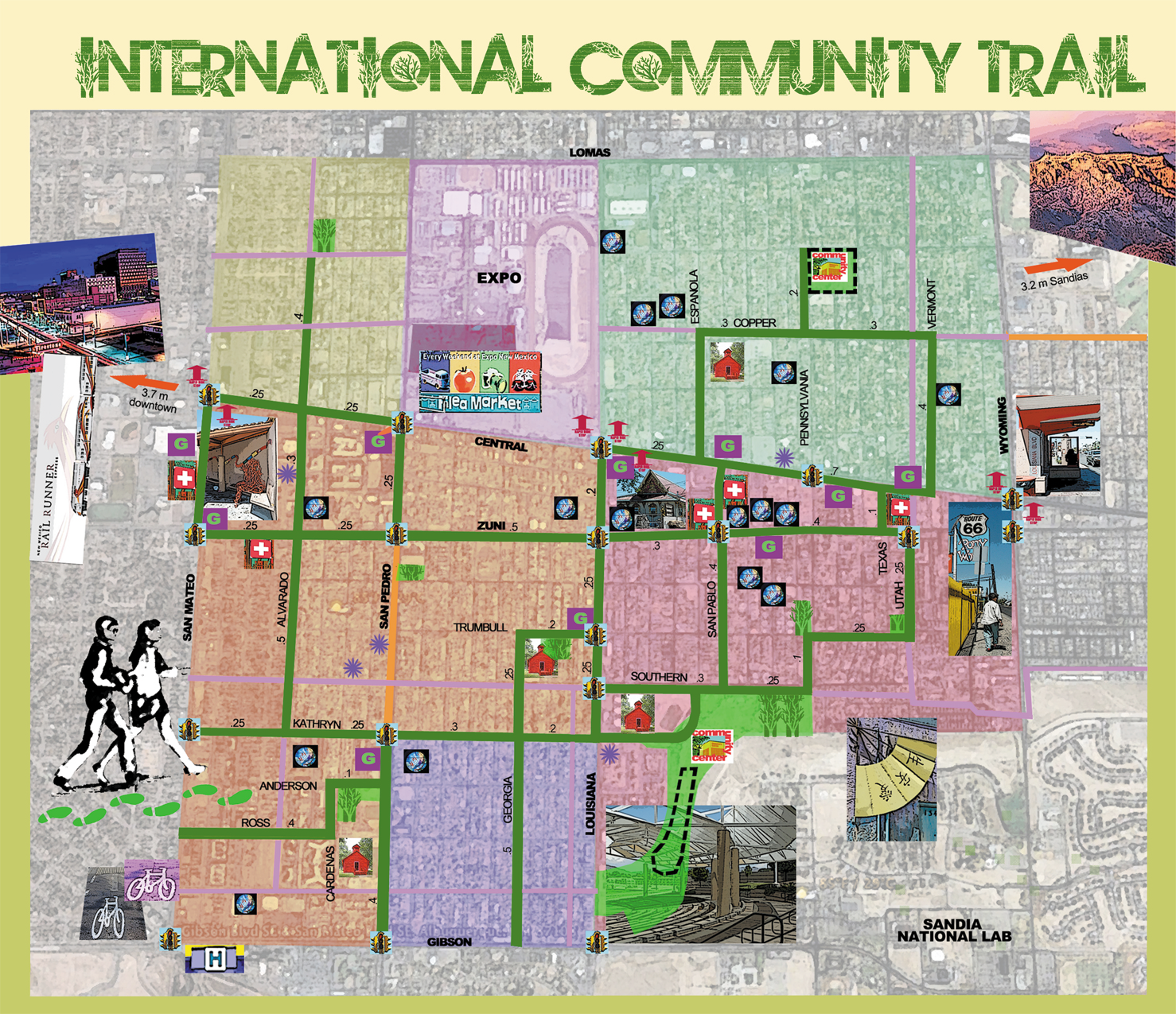
For example, in New Mexico HEROs work with local organizations around systems changes to address determinants of health, such as employment, transportation, food insecurity, etc. Below are some useful tools that HEROs have used or created as a way of providing technical assistance to communities. The first is a map of “food deserts” in New Mexico; the other a walking trail map developed for one of the most densely-populated zones in Albuquerque. Click on the thumbnail images for a larger view:
Other examples of technical assistance provided by health extension agents:
- help build capacity around grant writing and sustainability for community organizations
- assist with improving efficiency of practices and assist in the transformation process towards becoming a patient-centered health home
- help with the recruitment and retention of health professionals in rural and/or underserved areas
- help their communities identify and prioritize their health needs. Below are examples of county-level report cards created through health extension initiatives:
Training & Education
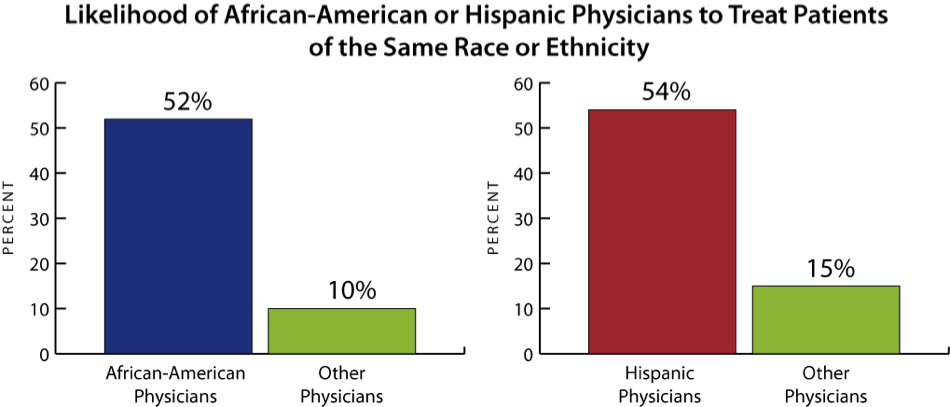
Health extension emphasizes “growing our own” workforce with regard to geographic locality and ethnicity as a strategy to address access to care. It is more likely that local trainees will be culturally competent and work locally. Black and Hispanic physicians are about 5 times more likely to care for patients of the same ethnicity, which demonstrates the need for “growing our own”.
Health extension agents help develop capacity for creating roles for and training community health workers. The following document may be useful in making the business case for community health workers (CHWs), key allies in community health improvement. Click here for more information on health extension and CHWS.
With an eye toward the broader role for front line, primary care practices in society, health extension has promoted training and education on the principles of the Ottawa Charter for Health Promotion and the World Health Organization’s primary care documents.
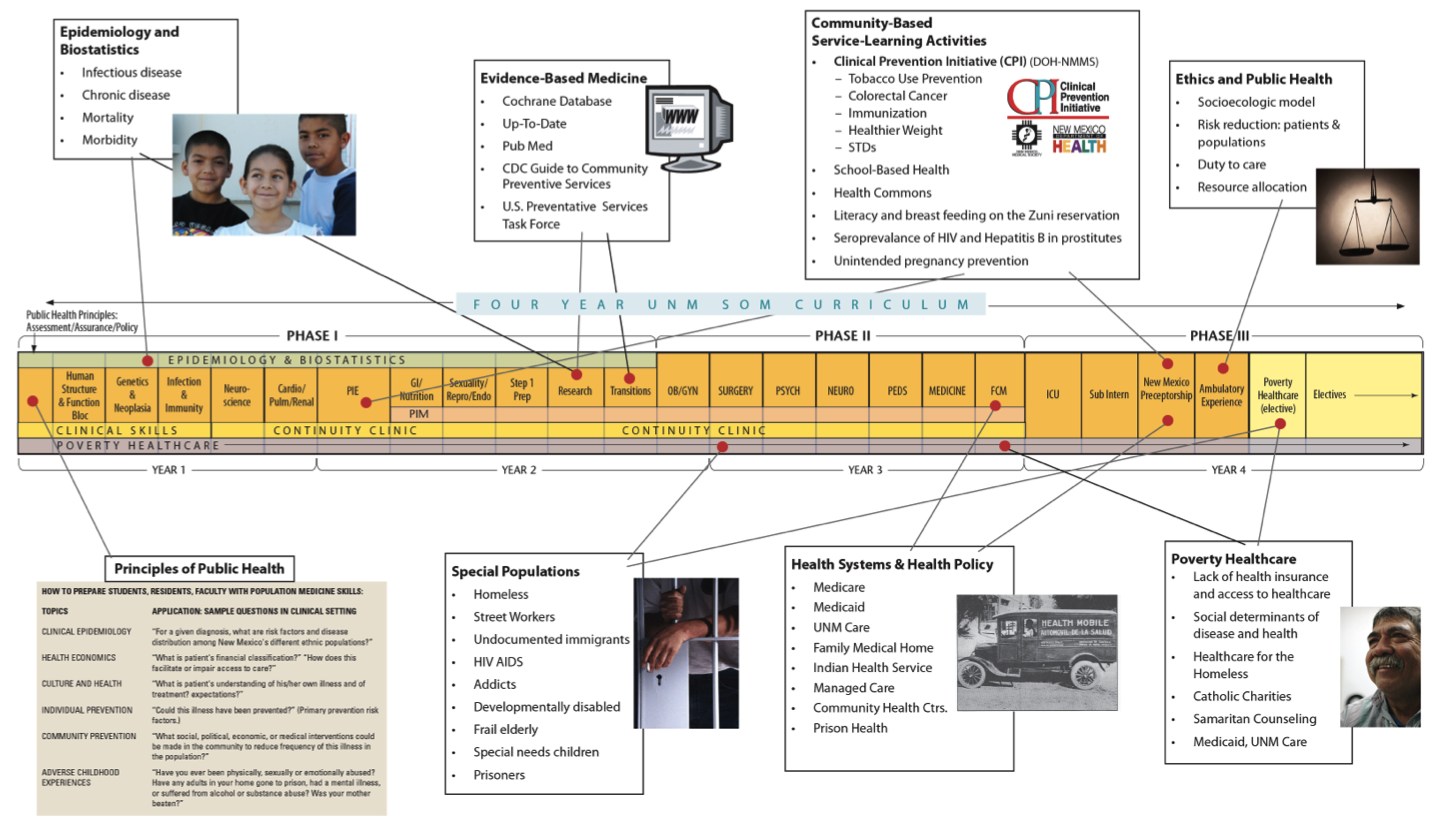
Broader skills for health professionals to address community health is embedded in UNM’s public health certificate, required for all medical students and family medicine residents. HEROs serve to link these learners to community groups and programs. Click below to view a timeline of UNM’s public health certificate program.
In the health system setting, health extension can:
- link clinic staff and providers to local schools and to local university students
- promote home visiting programs
- assist community hospitals in “community health assessments” and “community health improvement” as part of their community benefit requirement
- train medical staff and providers to work with communities
- train medical staff and providers to integrate public health into their medical services
- invite frontline clinic staff and providers to mental health first aid training
- create role in training CHW workforce linked to primary care practice
Health extension also has the potential to create a “learning community” helping individuals in professional positions who aren’t degreed in the field to move on to higher education and, ultimately, feel more secure in their positions with an ability to advance
Facilitation & Coaching
Practices have different needs and change at different rates depending on their readiness for change, history with change, and resources available, including staff and funds.
Practices are often so overwhelmed with patients and feel stretched in terms of staff and resources, so they need help and guidance–which EMR to choose? How to achieve meaningful use? How and where to recruit personnel? How to offer continuing education for their staff? How to keep current with the best evidence of practice when information overload is manifested by the growing pile of unread journals?…
Practices with change facilitators demonstrate significantly more capacity for change. Health extension can assist practices in their path to transformation in the following ways:
- Health extension offers help and offers objective, evidence-based approaches to practice needs and dilemmas
- Health extension is there for practices in the long haul, and can follow up on what technical assistance works, what doesn’t, and what has to be modified
- Health extension can link practices with community resources needed by patients but of which the practitioner may not be aware or know how to access
- Health extension can provide practices with “academic detailing”, a transformation pharmaceutical detailing which instead brings best practices & evidence-based interventions to practices (see below)
- Health extension can help gauge the help practices need and want
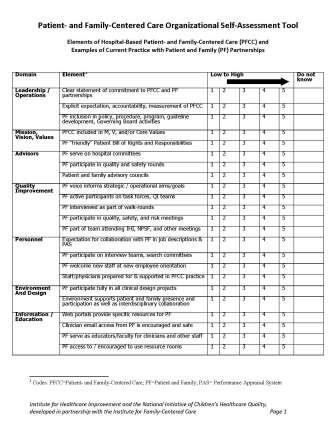
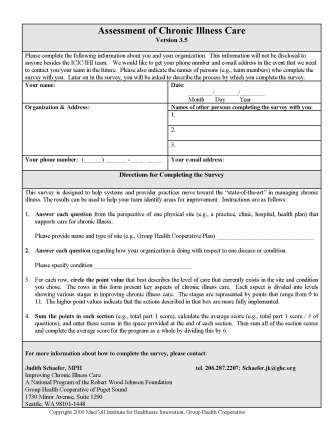
- Health extension can survey the practice regarding readiness for change and suggest where to start along the path to practice transformation. Below are some sample assessment tools:
Some of best approaches are “academic detailing”, an adaptation of pharmaceutical detailing which can be described as evidence-based detailing around best practices in primary care. This can transform and apply the most effective aspects of pharmaceutical detail agents in promoting to practices a number of new drugs produced by the parent company to the delivery of evidence-based approaches to practice.
Addressing Priority Health Needs
Health extension works with local communities to identify health priorities for their diverse populations, as well as deciphering methods for like-minded organizations to collaborate and share resources. They assist in cultural competency issues, provide training and presentations around the health needs of the populations they serve. HEROs also help communities access services, by linking them to shared resources.
An effective health system adapts to the ethnic, linguistic, or religious needs and economic and geographic circumstances of different populations in that service area. This can mean a recognition of dietary preferences, affordability of certain prescriptions, availability of translators and access to public transportation. Additionally, special populations like the blind, wheelchair bound, mentally ill or developmentally disabled require special physical and personnel accommodations. Health extension agents have helped their health system and communities adapt to these unique needs with some of these sample interventions:
- Offer help and offer objective, evidence-based approaches to practice needs and dilemmas
- Hold health career fairs targeted to specific populations– Blacks, Native Americans, Hispanics– conducted by recruiters with cultural sensitivity toward the experience of each group of students
- Identify health professional role models of different ethnicities and connect them with students as mentors
- Educate policy-makers, medical service workers, and public health staff on health and health equity
- Conduct community organizing for people in marginalized communities
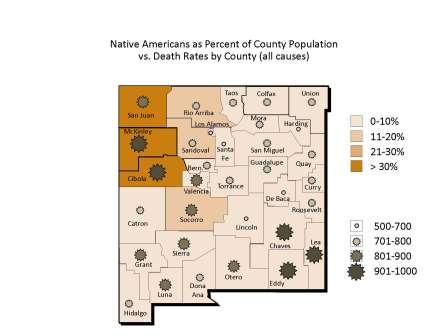
The interface between minority status and increased death rates is particularly apparent in New Mexico. Click on the image below to see maps correlating minority population density and high death rates by county:
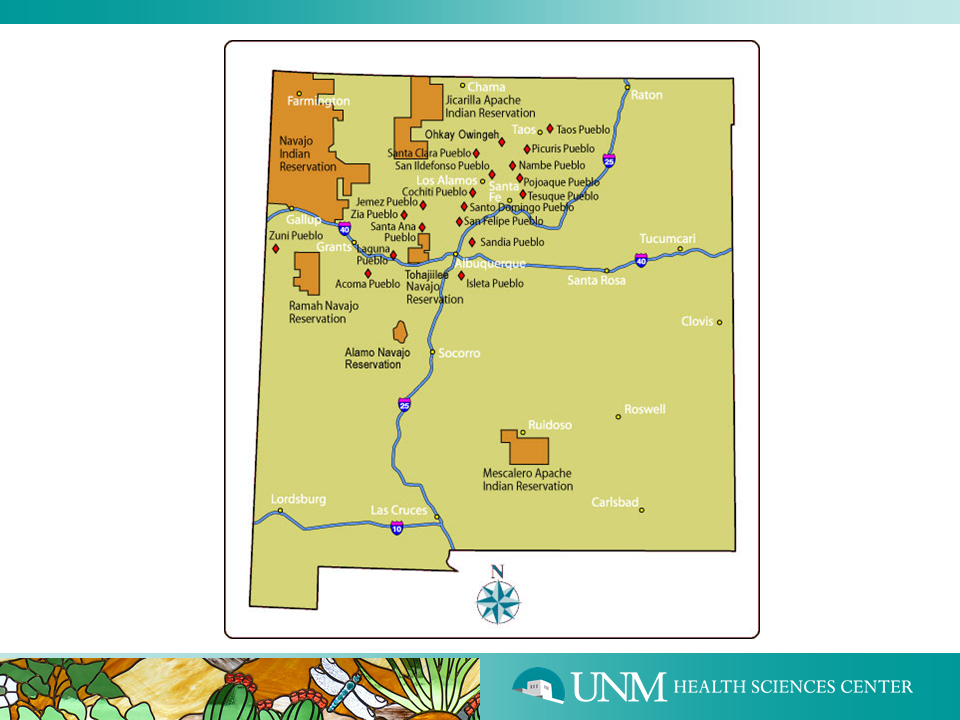
The Native American community on reservations face long travel distances to Albuquerque hospitals and specialists for care. Often, especially for elders, a Native liaison who is culturally competent is a necessary facilitator communicating treatment plans and follow up. In New Mexico, three Native American HEROs were hired and trained to provide this facilitating function for reservation-based Native patients.
Below is a map of the different Native American groups in New Mexico:
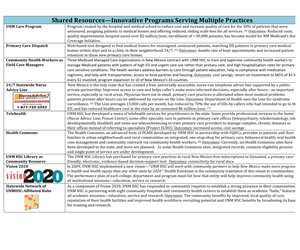
Linking to Shared Resources
Below is an example of the set of “shared resources” available in New Mexico:
Advocacy & Informing Policy
Health extension can train providers and staff on social determinants of health:
“Teaching critical health literacy in the US as a means to action on the social determinants of health”
Advocacy and informing policy can also take place at the grassroots level. Health extension agents mobilize and give health message training to those in the community who influence lay public: train groups of barbers, hair dressers and ministers on topics such as sexual violence, the need for diabetes and hypertension screenings, ways to offer patrons resource guides for area services. They also train community members in organizing, advocacy, mobilization and social networking.