Partnerships in Challenging Times
“Shared Resources” have become increasingly necessary, not only for small, independent practices, but for community organizations as well, leading to alignment of priorities and programming across the state. The University of New Mexico Health Sciences Center adopted their Vision 2020, which is “Partnering with communities, we will improve health and health equity more than any other state by 2020.” In order to reach this vision, the HSC has recognized that we must move beyond competition and better align our priorities, resources, and strategies in partnership with other people, organizations, and institutions in our state.

Vision 2020
 The UNM HSC Vision 2020 – “University of New Mexico Health Sciences Center will work with community partners to help New Mexico make more progress in health and health equity than any other state by 2020” came from the leadership of the HSC as a way to support the improved health of New Mexico communities.
The UNM HSC Vision 2020 – “University of New Mexico Health Sciences Center will work with community partners to help New Mexico make more progress in health and health equity than any other state by 2020” came from the leadership of the HSC as a way to support the improved health of New Mexico communities.
Vision 2020 creates the first academic health center strategic plan that focuses on improving a state’s population’s health and health equity as a measure of the institution’s success. To fulfill this Vision, all colleges, schools, departments and programs at UNM HSC have incorporated into their annual performance plans how their education, service and research enterprises will measurably improve the health of New Mexico.
The key behind Vision 2020 is learning as an academic health center to respond to the community priorities as opposed to our own. Also, through alignment of activities and strategies we can use resources more effectively and have a larger impact on community health. A major tool in accomplishing this vision is through the use of health extension. When the institution has a full-time staff person form the local communities who lives in the communities it serves it can respond more quickly and effectively to the needs.
This is part of a national movement for Academic Health Centers to measure their success by the health of the communities they serve. An institutional commitment through the adoption of the vision has been an essential piece of this goal, as well as the integration of this vision into the work of all the colleges, departments, and offices.
We will do this by focusing on evidence-based interventions and evidence-informed policy, by disseminating and building on successful programs and pilots, and by linking and aligning existing resources to address community priorities for improving health and health equity.
The terms “health equity” and “health disparities” are used frequently in our vision and in the reports; for clarification, “health disparity” is a difference between health outcomes between a persistently socially disadvantaged group and one that has a higher relative position in the social hierarchy. “Health equity” is the pursuit of the elimination of these disparities.
For more information, visit hsc.unm.edu/vision2020
Health Extension Hubs
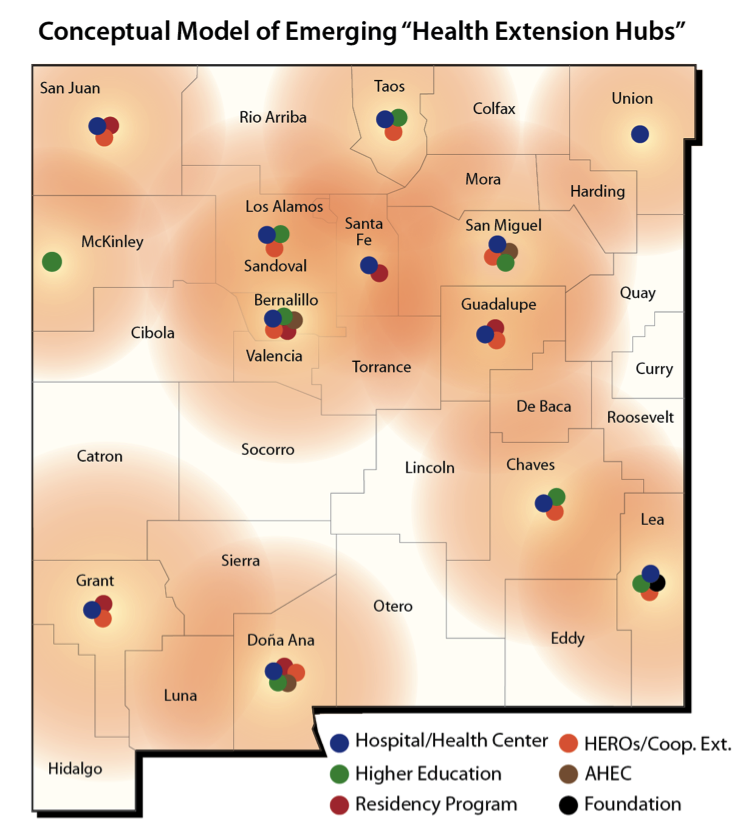
The University of New Mexico Health Sciences Center (UNM HSC)/Community Academic Extension Hubs refers to community-based organizations, institutions, or programs in a particular region that make an arrangement with UNM HSC to serve as a local extension of the HSC in areas of interest to them: education, service, research and/or policy.
The concept has grown out of lessons learned from different campus-community models—the agricultural Cooperative Extension Service, Health Extension Rural Offices (HEROs), rurally-based residencies, and memorandums of agreement between community hospitals or community health centers and UNM HSC. These models reflect the value of decentralizing the resources of UNM HSC to local communities to better response to community health priorities.
Creation of local Academic Extension Hubs facilitates community capacity-development in health through community access to numerous HSC resources in areas as diverse as pipeline development, workforce development, telehealth, clinical service improvement, community-based education, program evaluation and research. Having full-time, community-based, UNM HSC-affiliated personnel helps UNM HSC improve its knowledge of and response to community needs.
Finally, the development of Academic Extension Hubs is an important vehicle for helping UNM HSC fulfill its Vision 2020: UNM HSC will work with community partners to help New Mexico make more progress in health and health equity than any other state by 2020.
Examples of Successful Partnerships
Shared HERO Costs
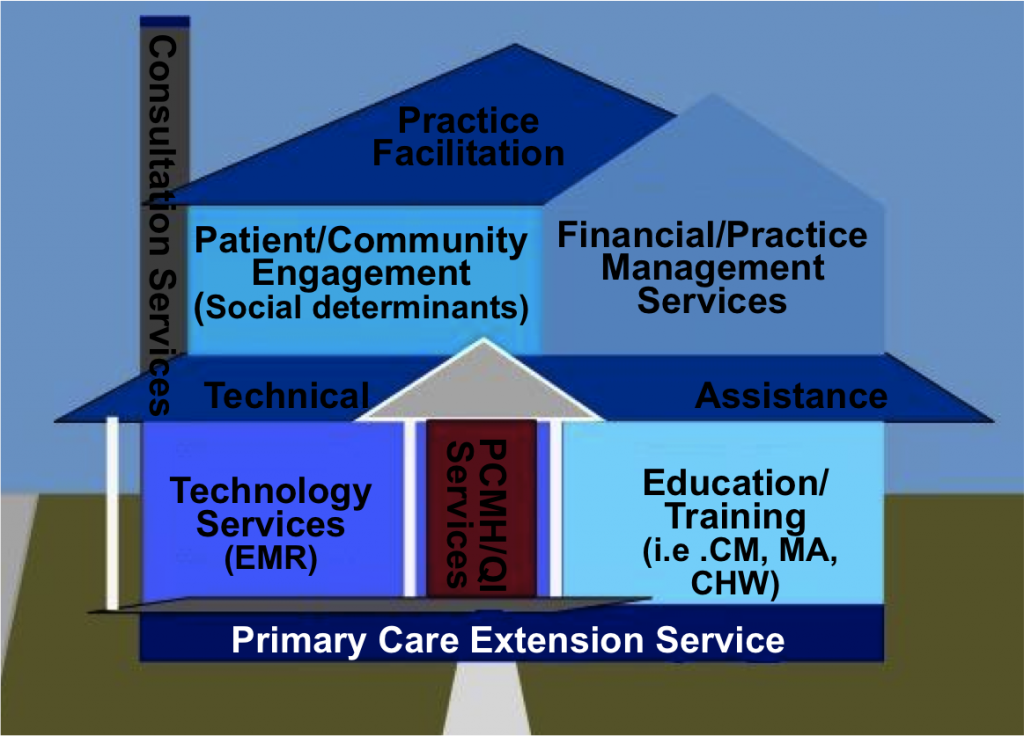
The funding for health extension, and in particular as it relates to primary care transformation, can also be visualized similarly to the payment system for utilities (water, sewer, electic/gas, etc). The graphic below demonstrates how a primary care extension service, when visualized as a shared “utility”, could support a whole range of activities in the improvement of primary care.