Determinants of Health: What is Making Us Sick?
Determinants of health in the most simplest terms are what make us sick or healthy. In looking at community or population health and going beyond the clinic walls social status, stress, childhood, social exclusion, work or unemployment, education, social support, addictions, food, shelter, and transportation are key determinants of health. These are often called social determinants of health.
Medical professionals and institutions are in a unique place to educate and advocate for everyone’s fair opportunity to access to these determinants. Improvements in these determinants will reduce the strain on our medical system. The Community-Centered Health Home Model, Community Health Report Cards, community level data collection and action, as well as partnerships are all examples of a determinants of health approach.
For Health Extension workers dealing with community or urban situations it is important to understand the concepts of structural determinants and intermediate determinants. Structural determinants of health are those that create the social hierarchy, such as income, education, gender, age, ethnicity, and sexuality. Intermediate determinants emerge from social stratification and creates differences in exposure to health determinants. These include living conditions, access to health care, access to education, and working conditions.
The Community-Centered Health Home Model
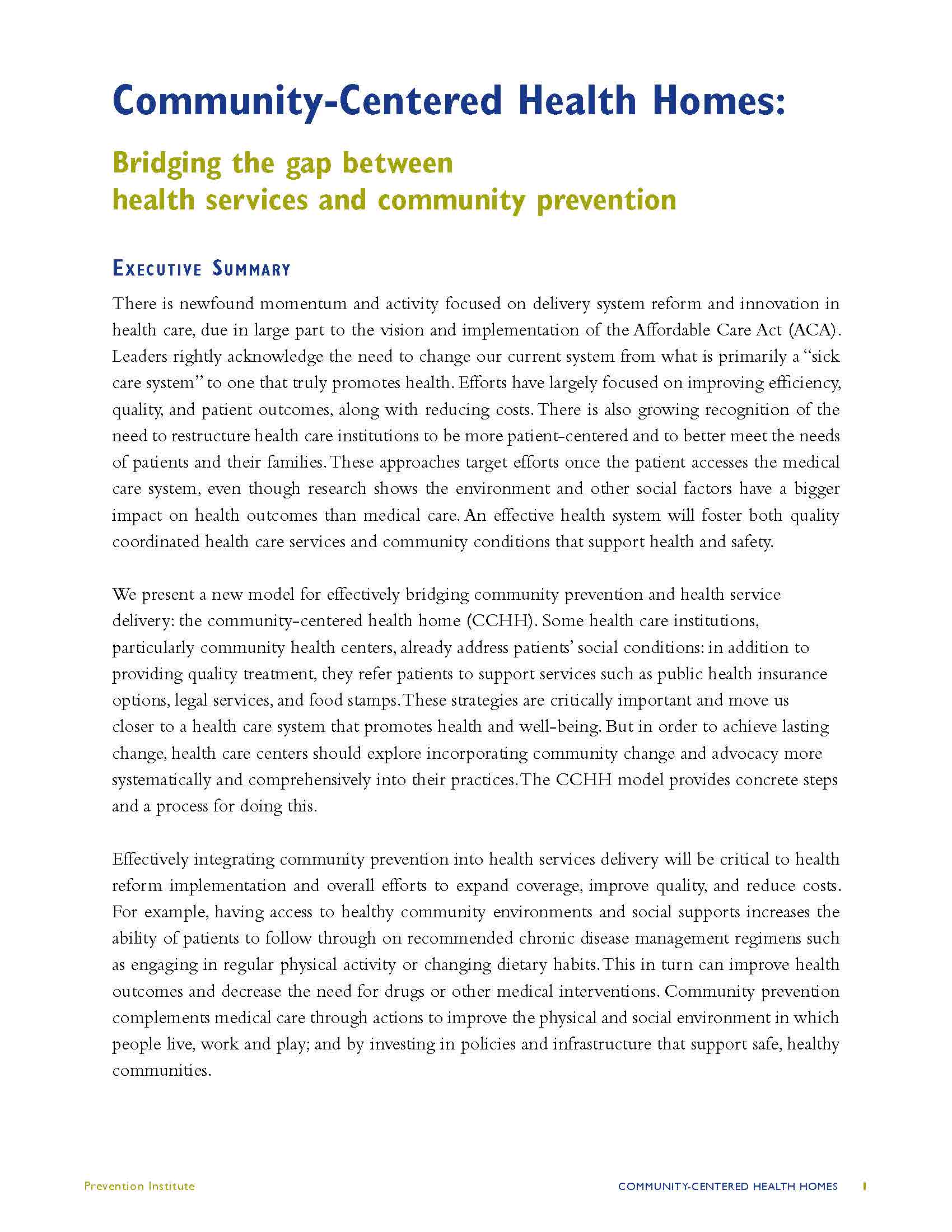 The Community Centered Health Home model, put forth by the Prevention Institute, builds on earlier health home models and innovative ideas like the Community Health Centers and the Primary Care Medical Home included in the Affordable Care Act. Essentially, the Prevention Institute argues that the concept of a PCMH needs to be expanded to include not only patients but the entire community in which patients live, work and raise their families. This nuanced model enhancement calls for providers to be responsible for quality health care delivery while also engaging and collaborating with the entities that address social determinants of health. This paradigm shift moves health care providers toward becoming part of the solution in addressing the social determinants of health and causes of health inequity.
The Community Centered Health Home model, put forth by the Prevention Institute, builds on earlier health home models and innovative ideas like the Community Health Centers and the Primary Care Medical Home included in the Affordable Care Act. Essentially, the Prevention Institute argues that the concept of a PCMH needs to be expanded to include not only patients but the entire community in which patients live, work and raise their families. This nuanced model enhancement calls for providers to be responsible for quality health care delivery while also engaging and collaborating with the entities that address social determinants of health. This paradigm shift moves health care providers toward becoming part of the solution in addressing the social determinants of health and causes of health inequity.
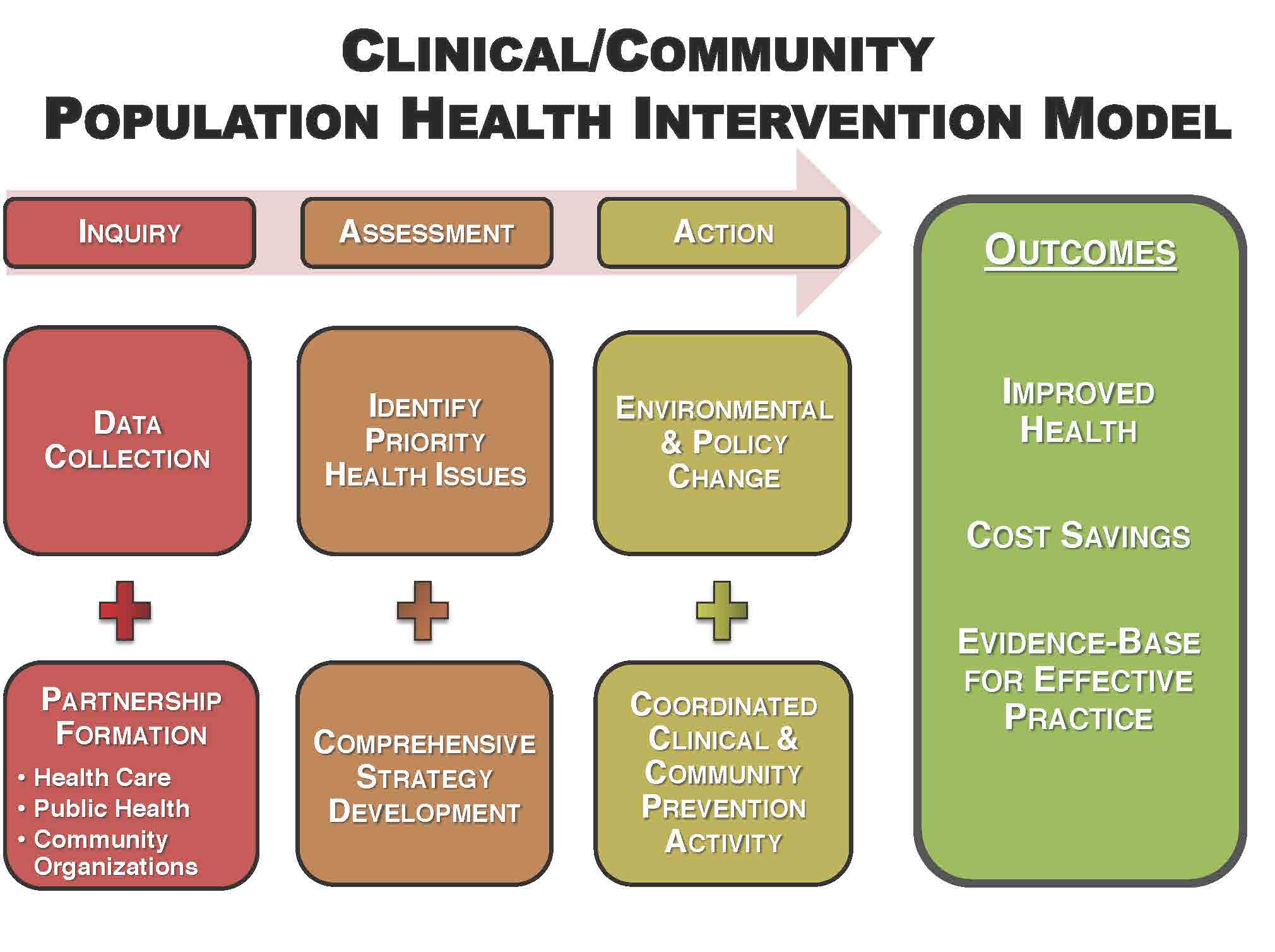
“Clinical/Community Population Health Intervention Model”
In outlining the model of a community health home, the Prevention Institute has identified the key elements leading to outcomes as:
Inquiry: Given the constant contact of health centers with patients in their surrounding community, they are uniquely positioned to maintain a “finger on the pulse” of their community’s health. To do this more effectively, they need to collect data that reflects community conditions, analyze medical records for community health trends, and capture clinician impression and intuitions about underlying issues shaping the prevalence of injuries and illness.
Analysis: Once health and safety information is collected, health centers can play a key role in identifying underlying problems and prioritizing possible solutions. Community centered health home staff would analyze the collected data and share it with community partners to jointly identify the factors in the community environment that are influencing health and safety outcomes.
Action: Given the credibility of medical professionals, clinical staff and health institutions can play critical roles in advancing broader systems change that improves community environments. Actions should be built on the evidence and partnerships that are developed in the analysis phase. Partners should include community residents and representatives from sectors outside of health that make decisions that impact, such as transportation, housing and agriculture.
Below is a visual representation of how community centered health homes extend the reach of a primary care practice into improving community health:
Community Health Report Cards
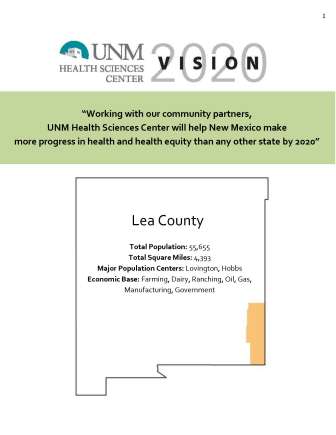
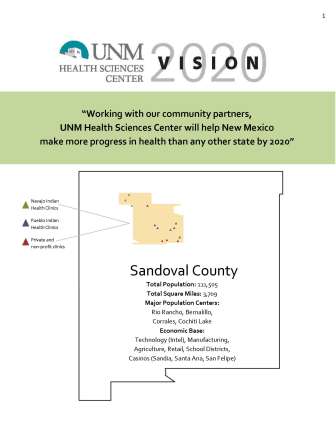
The Vision 2020 County Health Report Cards have been created to provide a resource to community partners as well as to inform Health Science Center (HSC) internally about the strengths and resources within our New Mexico counties.
In the report cards we provide selected contacts from the county that the HSC has relationships with and who represent many of the experts and leaders within the community. We also share general demographic information to provide context as well as information on licensed health professionals and some of the activities the HSC does in partner with communities in our mission areas of Education, Service, and Research. The report card highlights the priorities of the county as well as state-wide health priorities in order to guide the work of the HSC to meet the needs of the communities we serve.
The report card examines health outcomes and factors in relation to the other counties in the state. We also look at the health disparities in the county and state in an effort to understand how we can work towards our vision of “partnering with communities to improve health and health equity…”
The report concludes with a summary of the HSC Vision 2020 and identifies ways to partner to improve health in our communities. We identify some of the strategies the HSC is using to reach this vision through the leveraging of our resources to meet the needs of communities in the state including the use of the Health Extension model and the emerging Academic Health Hubs.
Using Community Data to Inform Services & Programming
The most concrete way to address the social determinants of health in service provision and programing is to be data-driven. In this manner, political grumblings reacting for or against barriers inherent in systems change efforts can often be diffused or eliminated by simply pointing to the data. In particular, use of data from reputable, nonpartisan sources is critical. The use of national data sets provides an overview of the specific catchment area and allows advocacy groups to situate their undertaking in a larger national context. Pairing national data with locally generated data from government and nonprofit or safety net organizations provides a more expansive view of what contributes to the social determinants of health in order devise a localized, workable plan of action with an attainable goal.
Community Partnerships for Health Improvement
Helpful tips from the trenches for working in a board-based collaborative effort:
- Expect the work to be political – that’s what advocacy is and systems change is long grueling work. Make sure that the leadership of the organization is prepared to address emerging conflict publicly.
- Keep the overarching goal center stage – “eyes on the prize.” This will keep the group focused and in support of each other as movement toward systems change may be arduous.
- A frank discussion of ownership of the effort needs to be addressed and official agreements made to avoid conflict. The tug o’ war that occurs between organization participating in a concerted, broad-based effort is often foiled by one of the partners claiming ownership of victories, demolishing established trust.
- Share openly with the other collaborators/stakeholders in the group the extent to which your organization can engage and why your participation at certain milestones in the systems-change movement may be limited.
- Have a local data expert on your team like an Epidemiologist from regional Department of Health and welcome students who are constantly digging into the most recent literature in order to stay relevant and course correct if necessary.
- If you don’t like the composition of an institution that is affecting the health of your patients/community members, use political will of mobilized group to change situation by supporting new candidates for electable positions.
- With diverse membership, group has a “pulse” on the community and organizations that can make a difference.
- Around the point of advocacy towards systems change, be transparent about steps your organization is taking toward the group’s goal. Seeing media spots touting the contributions and successes of the group, without giving due credit and being inclusive in moments to shine, could very well lead to the collapse of the consortium.
- Strong, open-minded leadership is essential. Find someone who will not waiver during political turns of tide and who can’t be fired.
- If members of the consortium want to take on a side or allied project related to the larger goal, have some “group think” and discussion time. This new direction may be complimentary to achieving set goal or the small group may break off. Accept that it is part of the process that groups will diverge.
- If the group is stagnating, consider a review of existing strategic plan to take stock in accomplishments and to gage where members want to move forward.
- Invite new members/organizations to come to meetings and spend time brainstorming the valuable ways that they can participate. Make this concrete so that they clearly see connection to advocacy movement.
NM Special considerations: A central theme in the CCHH is provider expansion past the clinic walls. This is especially challenging, if not impossible, in impoverished, isolated and/or remote areas. Simply put, clinics do not have the in-house resources to add an additional layer of productivity to the existing work. In diverging from the Prevention Institutes belief that physician or health care provider leadership is required to implement an advocacy campaign, this role is ideal for a HERO. A HERO can be the mechanism for extending outside of the clinic walls as they perform a capacity building function and are not required “own” the work. Implicit and explicit in the HERO role, is the acknowledgement that all stakeholders have an important part to play that is rooted in a skill set, social network and discipline of study that boosts the contributions of the collective whole.