What is a Community Health Worker?
CHWs facilitate access to services, improve quality, and reduce disparities by serving as ‘bridges’ between their communities and health/social service systems. CHWs build individual and community capacity by increasing health knowledge and self-sufficiency through activities such as: outreach, community education, informal counseling, social support, and advocacy. They provide practical services to individuals, families, and communities. CHWs can be found working in health and human service organizations, schools, faith communities, public health systems, and community health clinics.
In 2010, Community Health Workers obtained a unique labor classification, which is described below:
CHW Core Roles & Skills
Links to the studies:
Training & Certification
HERO Role in CHW Workforce Training & Integration into Care Systems
The health extension infrastructure in a state, and health extension agents themselves, can play a vital role in training a CHW workforce and advocating for integration of CHWs into care systems. Health extension agents can provide training on chronic diseases, setting up group visits in a practice led by CHWs, and cultural competency.
For example, in New Mexico, there was a need for increased CHW capacity-building on issues such as diabetes, medical terminology, cultural humility and other topics. These topics have been specifically requested by CHWs and CHW trainers based on special interest and specifically tailored to meet the needs and enhance their practice based on their scope of work of the CHWs. Health extension agents (HEROs) identified the gap, realizing that training should be culturally and linguistically tailored to the needs of the CHWs and their academic background and learning needs as non-traditional adult learners. Through the use of technology and considering the budget constraints, CHWs from various rural and urban communities connected via telehealth to receive the training from HEROs, leading to increased capacity among the various groups of CHWs statewide. HEROs continue to offer ongoing trainings to keep this workforce updated, as well as offer trainings based on needs that arise at the CHW and community level.
I-PaCS: Integrated Primary Care and Community Support
CHW Collaborations in Research, Education and Service
The following are priority areas CHWs can address for Medicaid Managed Care members:
- Poverty
- Health literacy
- Transportation
- Food
- Housing
- Training
- Jobs
- Assistance with enrollment in entitlement programs
- Lack of funding for such services as literacy classes, GED, ESL
- Gas for transportation
- Behavioral health
- Knowledge of how to navigate health system
- Chronic disease education (ex. asthma, diabetes)
- Access to local physicians
- Time constraints interfering with prioritizing appointments
- Medication needs
- Utility assistance
- Support for substance abuse
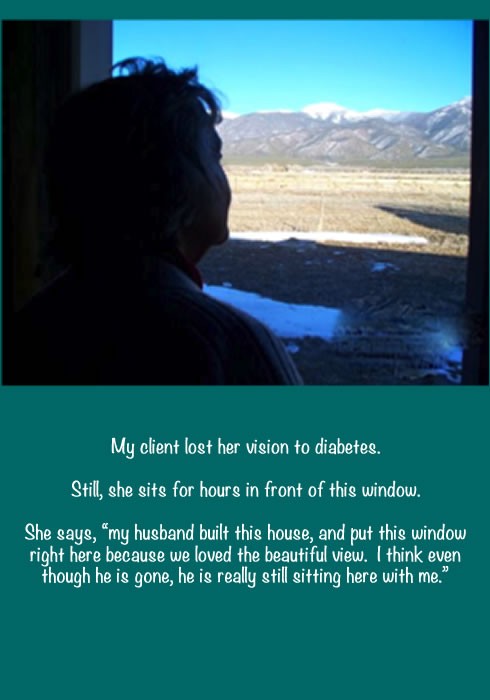
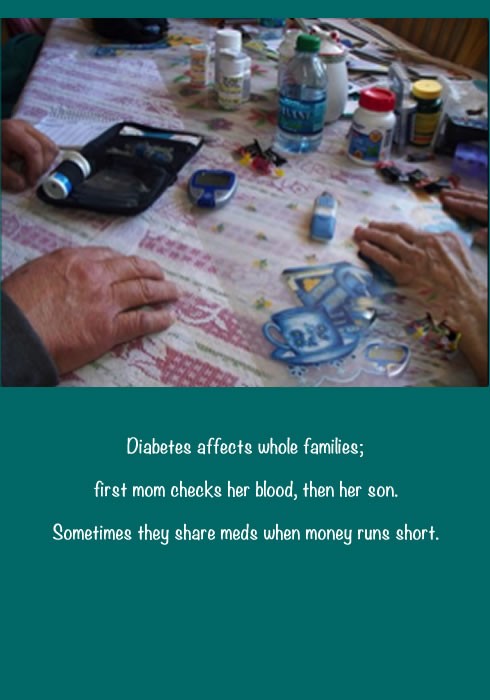
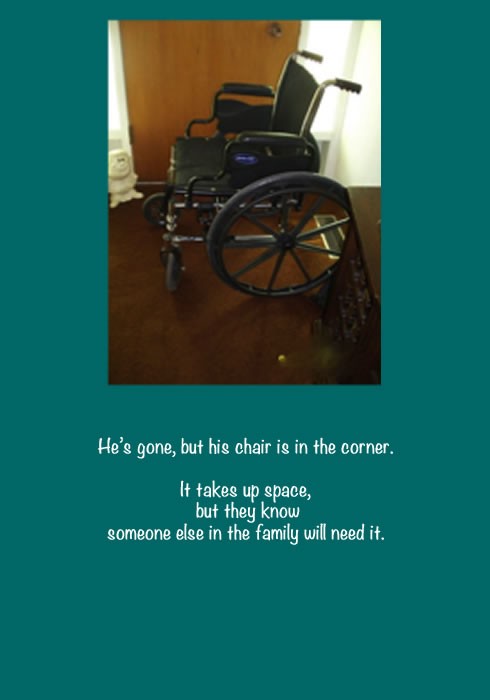
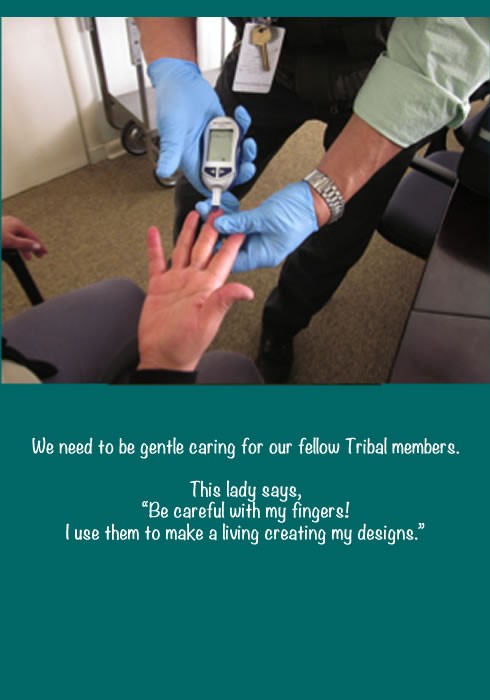
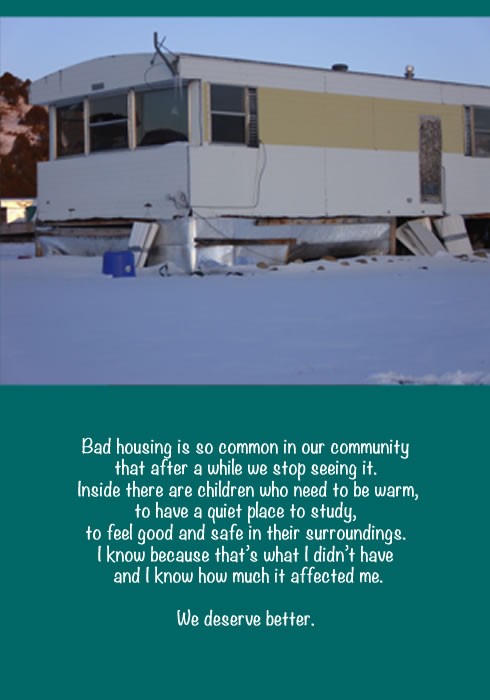
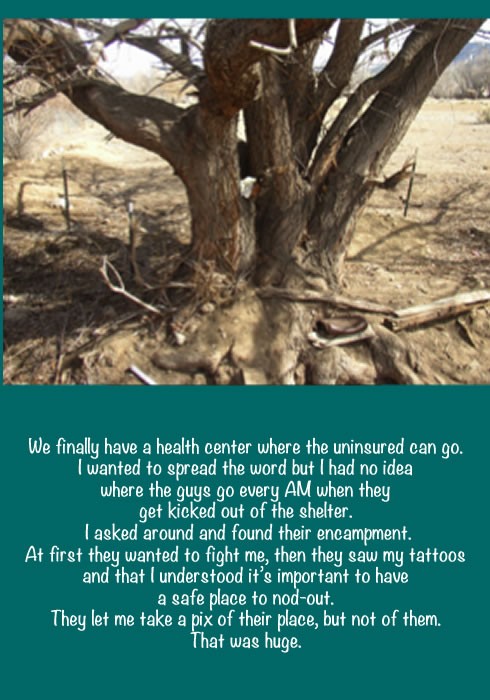
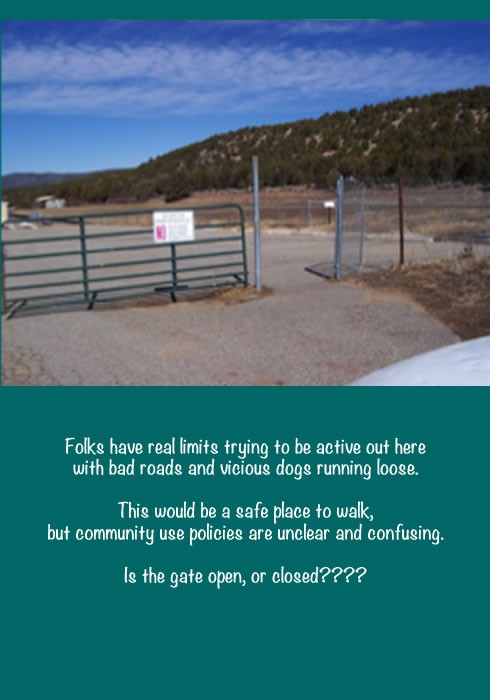
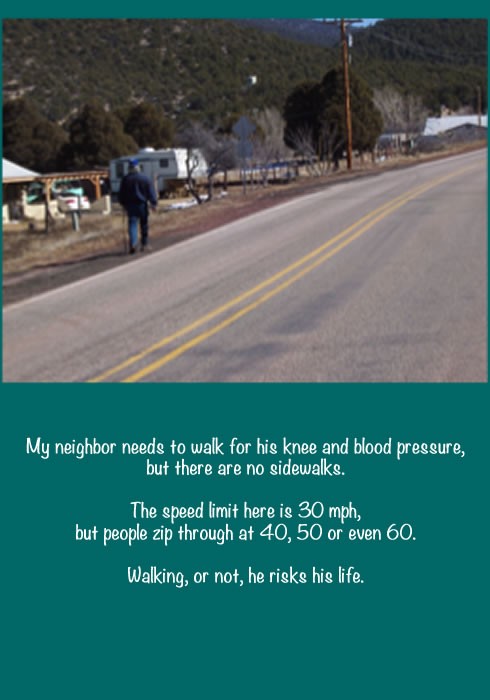
Stories of CHWs: A Photovoice Project
The following “photo voice” project was developed by community health workers participating in a two-semester-long course at the Taos branch campus of UNM. CHWs taking the course were given cameras and asked to take pictures that told the stories of their communities, as well as to describe what they saw occurring in the photos: