Health Extension as a Vital Resource for Managed Care Organizations & Health Centers
Click on the image below to learn more about the Expanded Chronic Care Model:
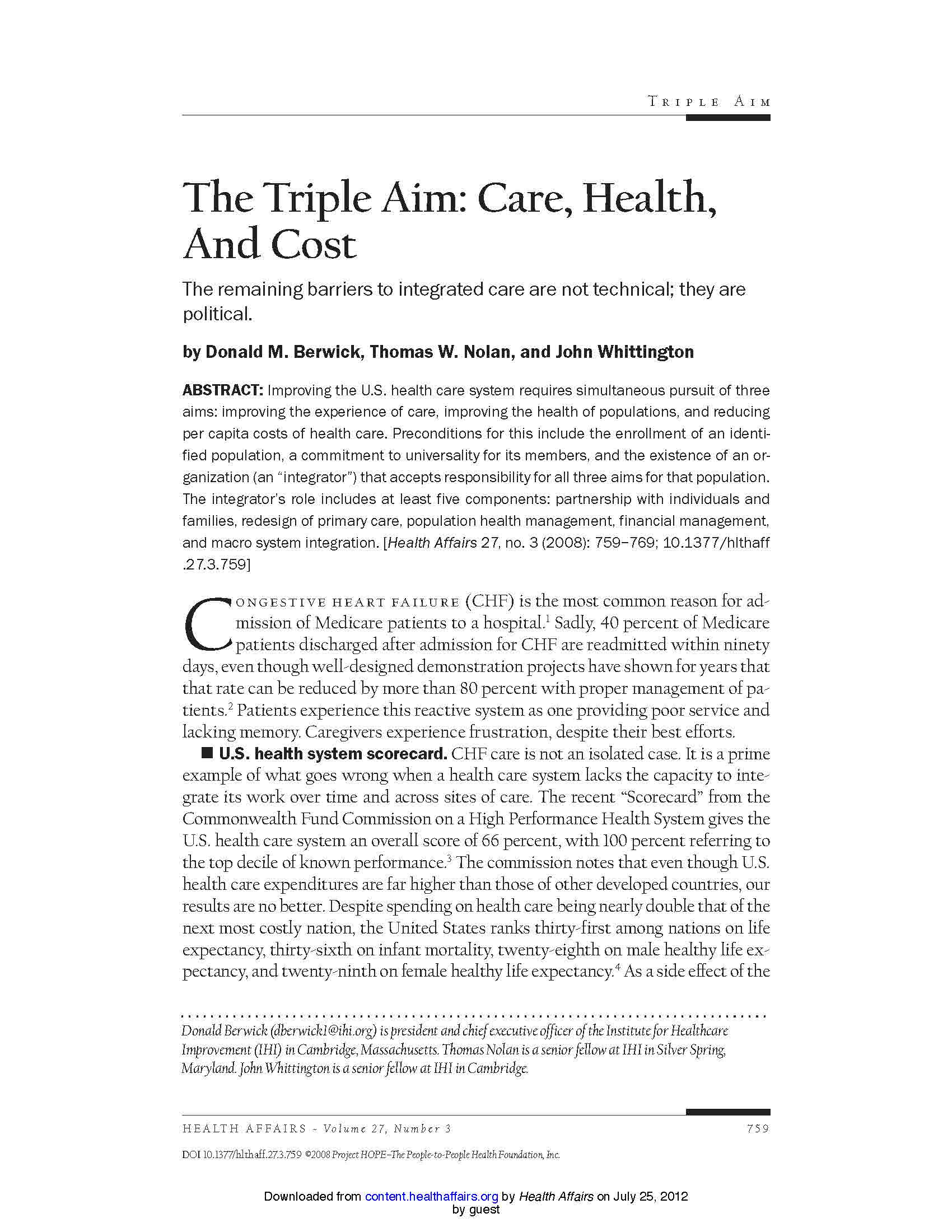
Triple AIM
D. Berwyk in JAMA November 24, 2010
 The Triple Aim initiative calls for redesigning the health care delivery system to simultaneously accomplish 3 primary objectives: improve the health of the population, enhance patient care (including quality of, access to, and reliability of care), and reduce or at least control the per capita cost of care. Triple Aim builds off the Institute of Medicine’s 6 aims for improvement in the delivery of health care in the United States as outlined in a 2001 report, “Crossing the Quality Chasm: A New Health System for the 21st Century”.
The Triple Aim initiative calls for redesigning the health care delivery system to simultaneously accomplish 3 primary objectives: improve the health of the population, enhance patient care (including quality of, access to, and reliability of care), and reduce or at least control the per capita cost of care. Triple Aim builds off the Institute of Medicine’s 6 aims for improvement in the delivery of health care in the United States as outlined in a 2001 report, “Crossing the Quality Chasm: A New Health System for the 21st Century”.
More information on the Triple AIM can be found using the links below, as well as in key articles found in “Related Literature and Tools”, below.
Diffusing Innovation among Health Systems & Payors
Innovative Health Systems Supported by Health Extension
 UNMHSC and its community partners who created the HERO program came together to develop an advanced medical home model over five years ago. The “Health Commons” model provides patients and their families in either urban neighborhoods or rural communities with an integrated, one-stop-shop for primary care, behavioral health, oral health, case management, public health, and enabling services via community health workers or “promotoras” working back-and-forth from the clinic setting to community. Currently, six Health Commons exist in the state, and more are planned. Each integrates programs around local data- identified health issues and priority community needs while contributing to local economic development by way of hiring and building capacity among community members.
UNMHSC and its community partners who created the HERO program came together to develop an advanced medical home model over five years ago. The “Health Commons” model provides patients and their families in either urban neighborhoods or rural communities with an integrated, one-stop-shop for primary care, behavioral health, oral health, case management, public health, and enabling services via community health workers or “promotoras” working back-and-forth from the clinic setting to community. Currently, six Health Commons exist in the state, and more are planned. Each integrates programs around local data- identified health issues and priority community needs while contributing to local economic development by way of hiring and building capacity among community members.
Related Literature & Tools
“The Triple Aim Journey: Improving Population Health and Patients’ Experiece of Care, While Reducing Costs”
Useful Tools:

“THRIVE Tool”
THRIVE is a tool to help you understand and prioritize the factors within your own community that can help improve health and safety. The tool can help answer questions such as: How can I identify key factors in my community and rate their importance? How are these factors related to health outcomes? What can I do to address each factor? Where can I go for more information?

“Improvement Tracker”
The Improvement Tracker allows you to track any of the measures currently available in the Topics area of IHI.org. Just select the measure you want to track (or create your own custom measure), set your aim, and enter your data. The Improvement Tracker automatically graphs your data. It lets you create reports, and even customize them for various audiences — your team, your CEO, your community.