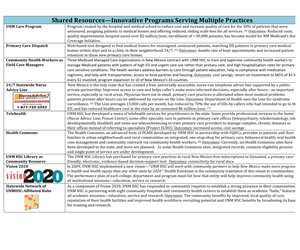
What are Shared Resources?
 In New Mexico, the HERO program decided to approach practices in a “demand” rather than “supply” mode—what did the practices actually need to improve their quality and contribute to their communities’ health instead of limiting what HEROs offered practices to a set of pre-conceived resources. Such open-ended inquiry led to a much broader set of needs and requests. Here are some examples: A way to get unassigned University Hospital ED patients assigned to a community practice; Help in recruiting physicians and mid-levels; Help in tracking patients referred to UNM HSC for which no information returned to the practice; Help in accessing the medical library and in receiving CME credits; Help in identifying health educators, especially diabetes educators to run groups in the practice; Help in writing grants to support practice innovations; Help in identifying epidemiologic help in evaluating and reporting on clinical programs the practice had developed.
In New Mexico, the HERO program decided to approach practices in a “demand” rather than “supply” mode—what did the practices actually need to improve their quality and contribute to their communities’ health instead of limiting what HEROs offered practices to a set of pre-conceived resources. Such open-ended inquiry led to a much broader set of needs and requests. Here are some examples: A way to get unassigned University Hospital ED patients assigned to a community practice; Help in recruiting physicians and mid-levels; Help in tracking patients referred to UNM HSC for which no information returned to the practice; Help in accessing the medical library and in receiving CME credits; Help in identifying health educators, especially diabetes educators to run groups in the practice; Help in writing grants to support practice innovations; Help in identifying epidemiologic help in evaluating and reporting on clinical programs the practice had developed.
How Shared Resources Address the Struggles of Small, Independent Practices
Examples from NM: Shared Resources for Practices
Complementing the state’s IT Regional Extension Center: New Mexico’s program decided to complement rather than duplicate other state-wide resources assisting primary care practices. LCF Research, the non-profit research entity to which the New Mexico state government assigned to apply for and run the state’s Health Information Exchange and its Health Information Technology Regional Extension Center offers all primary care practices and community hospitals assistance in selecting an appropriate electronic health record and its meaningful use. Successful completion of these steps enables each practitioner to receive $40,000 to $60,000 for adequate adoption of this technology in their practice. LCF Research, however, recognized that for more extensive practice transformation consistent with the primary care objectives of the ACA, small practices needed assistance beyond the technological improvements. They called upon HEROs to expand this service.
Insights from Pennsylvania
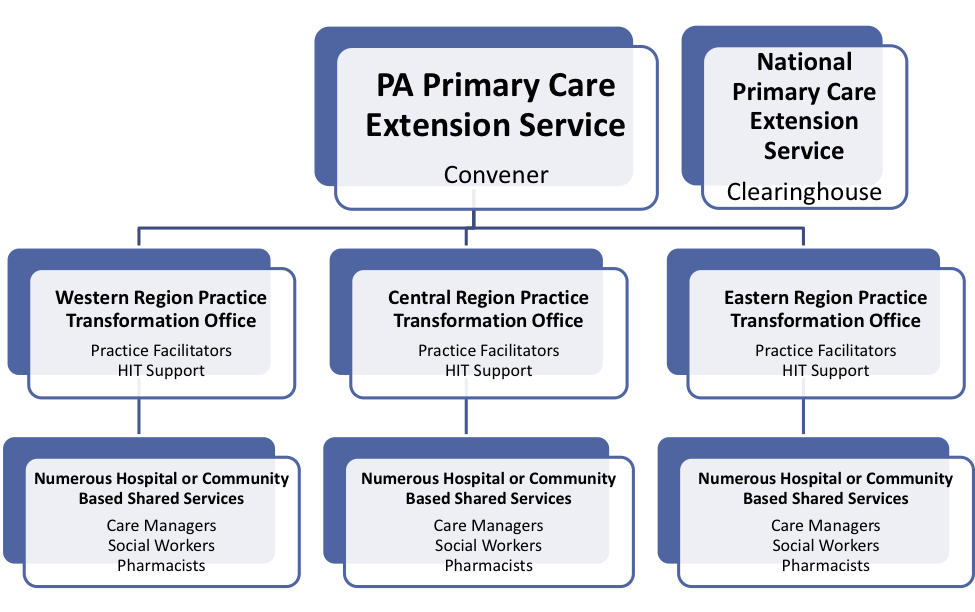
While Pennsylvania has numerous technical assistance providers and some initial local development of shared services to support smaller practices, no one has worked to foster collaboration and shared learning across these initiatives. That “Clearinghouse/Convener” role is seen as a key role for the Primary Care Extension Service in PA. For the past year, there have been quarterly partner meetings including representatives from government, health systems, payers, the state REC, provider organizations, and other stakeholder groups. They have also begun convening practice facilitators throughout the state to better learn what “facilitation” looks like in Pennsylvania and to begin to share best practices.
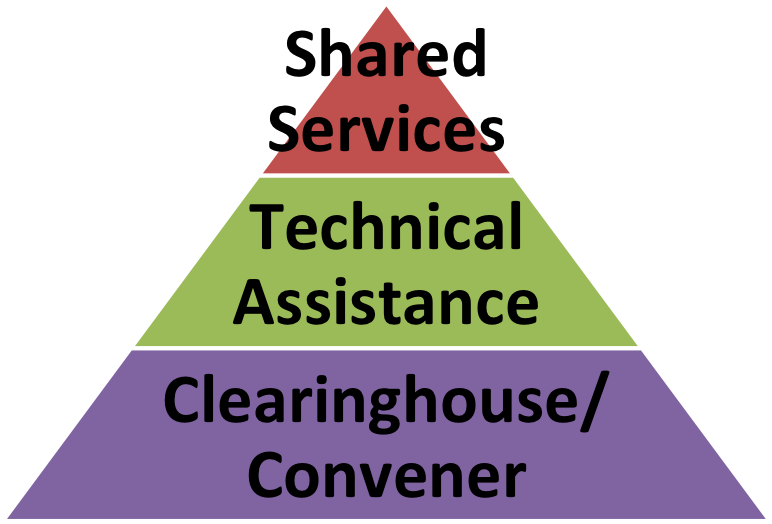
Over time, and as needs are identified, it is possible the Primary Care Extension Service may provide more direct technical assistance and shared services for practices and health systems. It also is possible that the Primary Care Extension Service formalizes a collaborative regional infrastructure and looks something like the following: